

Date: Tue, 16 Nov 2004 09:57:29 -0800
From: Chip Routt
Subject: Pelvic + Acetabular + Femoral Head/Neck Injury
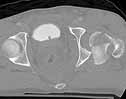
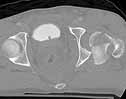
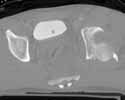
Here are some interesting plain films and CT images for a 22 yo male involved in an auto accident who was then struck as a pedestrian when he exited the vehicle.
 |
 |
 |
 |
 |
 |
He has a left sided sacroiliac injury with an associated posterior iliac fracture, femoral head fracture, femoral neck fracture with extruded head-neck fragment, and posterior wall acetabular fracture with osteochondral impaction.
He arrived at Harborview 20 hours after injury.
His overall medical condition was stable, he was awake and alert, and his pelvic ring mechanical exam was without instability. His left lower extremity nerves seemed to function well and he had normal peripheral pulses. His lab parameters were fine.
A manipulative attempted closed reduction of the left hip injury using adequate intravenous sedation and fluoroscopy guidance failed to alter the hip s radiographic appearance.
The case is open for discussion.
Chip
M.L. Chip Routt, Jr.,M.D.
Professor-Orthopedic Surgery
Harborview Medical Center
Seattle, WA 98104-2499
Date: Tue, 16 Nov 2004 15:47:08 -0600
From: Adam J. Starr, M.D.
Hi Chip,
That's a heck of a case.
I would vote for a KL approach. I think I could get access to the neck fracture that way, and should be able to reduce the head fragment into the joint. I'd plan to stabilize the nexk fracture with 6.5 screws. Since it would be an open reduction, I don't think cannulated screws would be needed.
I do my Kochers lateral - I know y'all do them prone in Seattle. I'm not sure which would be better in this case, but my instinct would be to do this the way I do most of them - so, lateral position.
I think I would try to fix the posterior ring injury with an iliosacral screw, placed with the patient in the lateral position. I think the ring injury can be stabilized with a screw into S1. I think the reduction of the ilium will require a push, from lat to med, but hopefully it'll go. Getting AP, inlet and outlet views is tough with the patient lateral, but it's do-able.
If the wing wouldn't reduce, then an open approach posteriorly (as you've described) would also work. I think you do those prone, right? - so, in that case, maybe a prone position for the whole shebang might be the best bet? Approach the hip via a prone Kocher and also do the approach to the posterior portion of the wing thru a separate incision? If you're in Seattle and all.
That's a real bear. What'd you do?
Adam Starr
Dallas
Date: Tue, 16 Nov 2004 15:37:37 -0800
From: Chip Routt
I'll wait for more discussion.
Don't forget that he also has a large caudal, anterior femoral head fracture.
Thanks for your comments-
Chip
Date: Wed, 17 Nov 2004 06:09:16 -0600
From: Adam J. Starr, M.D.
... he also has a large caudal, anterior femoral head fracture
I think I would see what I could see (and feel) from the back, around the bottom of the neck, and if I was unhappy with it I'd do a troch osteotomy.
I like an osteotomy better than a troch slide (or wafer - "digastric "? isn't that what the word is?) but I think either would offer access to the anterior aspect of the joint.
Adam
Date: Wed, 17 Nov 2004 07:02:56 -0800
From: Chip Routt
Thanks Adam.
Could you explain why ... "I like an osteotomy better than a troch slide"...?
Have you used both, and if so what led you away from one and toward the other?
Chip
Date: Wed, 17 Nov 2004 16:06:01 -0600 From: Adam J. Starr, M.D.
Howdy Chip,
Yes, I've used both, and I always seem to be able to see better with the osteotomy as opposed to the slide. It seems to me that the retraction of the abductors is better when the troch is freed up from its distal attachments. I'm better able to swing the abductor muscle mass up and forward to expose the bone above and forward of the tab.
But, maybe I'm not doing the slide right or something. Alan Jones here prefers the slide, I think. I know people who use the slide like it.
Adam
Date: Wed, 17 Nov 2004 14:51:44 -0800
From: Chip Routt
Do you have concern about trochanteric osteotomy fixation when considering the implant(s) for the neck fracture? Will they obstruct/complicate the osteotomy fixation?
Chip
Date: Wed, 17 Nov 2004 16:59:44 -0600
From: Adam J. Starr, M.D.
I use 3.5mm screws to repair the osteotomy, so I'd think I could manage to place them around the 6.5mm screws used to repair the neck fx.
Adam
Date: Tue, 16 Nov 2004 20:19:20 -0600
From: Andrew H. Schmidt
My approach would be a Smith-Petersen to reduce and fix both the femoral head and neck fractures ASAP. It's hard to tell now whether the neck is best fixed with screws or a DHS, but at first screws would suffice. The posterior wall and posterior ring can wait if needed.
Second stage (the same day or a later OR session) would be prone. First, I'd do a Kocher and fix the posterior wall, and convert the femur to a DHS if the fracture pattern indicated. Then, I'd do an open posterior approach to the SI joint and reduce and fix it with iliosacral screws.
If one wished, I suppose the SI joint could be fixed from the front, probably at the same time as the Smith Pete - essentially extending it into an iliofemoral approach. Advantages of this would be less risk of posterior skin problems from combined Kocher/posterior ring approaches on the same side. Disadvantages of this approach are a more difficult reduction of the SI joint and more difficult and less secure fixation.
Andy Schmidt
Date: Wed, 17 Nov 2004 07:32:07 -0800
From: Chip Routt
Thanks Andy--
Why to you recommend ASAP timing?
How do you sort out whether to use a DHS or screws for a horizontal mid-neck fracture?
Could you explain why you believe the anterior SI reduction is more difficult and the fixation less secure?
Have you seen skin problems when a KL and dorsal posterior ring exposures have been combined?
Thanks -
Chip
Date: Wed, 17 Nov 2004 12:46:20 -0600
From: Andrew H. Schmidt
Why to you recommend ASAP timing?
---Just a "gut reaction" to a displaced neck fracture in a young patient, but this is not a middle of the night case either. I would try to get to the neck/head fractures during daylight hours as soon as the patient was otherwise cleared for surgery. I wouldn't wait for a merely "convenient" time.
How do you sort out whether to use a DHS or screws for a horizontal mid-neck fracture?
--Imaging with the fracture reduced (this would have to be done intraoperatively). If everything was going to be done in the same OR session, and the fracture was vertical or base of the neck, I go ahead and use a DHS and extend that incision for the acetabulum after repositioning. If the posterior surgery were to be delayed, I would use percutaneous screws for the initial fixation and convert to a DHS at the time of the Kocher approach, so I wouldn t have to operate through a recent incision.
Could you explain why you believe the anterior SI reduction is more difficult and the fixation less secure?
--Limited exposure of the sacral ala leaves little room for reduction tools and fixation, plus with the patient supine the deformity is not reduced. It s also a comfort factor for me as I am far more comfortable doing this from the back. However, two anterior SI plates could be sufficient if you re good at this approach.
Have you seen skin problems when a KL and dorsal posterior ring exposures have been combined?
--Not specifically, but it's still okay to be nervous about it, especially if there was any sign of closed degloving.
Andy
Date: Wed, 17 Nov 2004 05:09:44 -0800
From: Solberg, Brian, M.D.
Chip:
Certainly a very difficult problem in a very young patient. I think the patient would be best served by a single approach to fix both problems. Our experience with combined head and neck fractures has been that the acetabular fracture is cephalad, peripheral and small; I think many could argue that they may not need to be fixed once the head fragment has been accurately reduced and fixed. In this case, your acetabular fragment is pretty big and displaced, mandating a formal open reduction
I think a Smith-Petersen approach, although pretty simple for the head/neck fracture is attractive, is inadequate for the tab. There's just no way to get around to that part of the acetabulum, get an accurate reduction and place hardware without significant chance of iatrogenic injury. Likewise a dual approach would completely devitalize the head and most certainly lead to AVN.
The data I have seen on using a KL approach for combined injuries is discouraging at best. Jim Stannard's meta-analysis demonstrated a 3 times higher relative risk of AVN using this approach for Pipkin IV fractures. The size of the capsulotomy needed for accurate reduction of the head/neck fragments is extensive and puts the ascending branch to the head at risk. Moreover, I don't think you can visualize and reduce the antero-inferior head fragment from the posterior side without dislocating the hip. So I would vote no here as well.
We have been using a surgical dislocation with digastric troch osteotomy on our Pipkin's for the last couple of years as Adam suggested. The anterior capsule is a gimme, so use this to get a good exposure of the head and neck fragments for reduction and fixation first. I think the only shot this guy has is with an anatomic reduction of the neck and head. For the PW, I don't take down the short external rotators unless I have to, most of the time the PW fragment is cephelad enough to avoid this. By doing this, at least in my mind, I think I avoid any direct or indirect trauma to the ascending branch by steering clear of its path. Although the European literature is pretty rosy on using this approach (0 cases of AVN in 28 pts) our experience is more in line with using a Smith-Pete approach (1 AVN in 10 pts). Good luck!!!
Brian Solberg, MD
Cedars Sinai Medical Center
Los Angeles, CA
Date: Wed, 17 Nov 2004 15:54:16 -0600
From: Adam J. Starr, M.D.
I would use a lateral position, and I would fix the posterior ring injury. I think that would help the patient.
There's no question that imaging a laterally positioned patient is hard - the tech has to move the base of the C-arm up and back to get inlet and outlet views. But, it is do-able, and would likely be faster than re-positioning the patient.
I think you could avoid lateral positioning altogether if you were willing to do the Kocher prone - but, I never do them prone, and I wouldn't want to do my first prone kocher on a tough case like this one.
Date: Wed, 17 Nov 2004 07:10:50 -0800
From: Chip Routt
Thanks.
Can you explain for us why... "a dual approach would completely devitalize the head and most certainly lead to AVN".
Maybe you could comment on the dual approach dissection details which would cause femoral head death?
Do you think any soft tissue attachments remain on the extruded head-neck fragment? Any on the anterior inferior head fragment?
Would you discuss the imaging details with the patient laterally positioned? Do you use imaging intraop?
Thanks-
Chip
Date: Wed, 17 Nov 2004 07:54:01 -0800
From: Solberg, Brian, M.D.
Chip:
1. Literature is sparse but dual approach in Marchetti's (J Orthop Trauma. 1996;10(7):455-61) small series of Pipkin IV's was associated with a 5 fold increase risk of AVN. Swiontkowski (J Orthop Trauma. 1992;6(4):437-42) also found a much higher relative risk with dual vs anterior or posterior approach. Although I'm not certain, near circumferential capsulotomy certainly plays a role. I have no data to back this claim up.
2. I don't know if the neck has any attachments left but the antero-inferior head fragment usually retains capsular attachements. Because you cant be sure I think you have to try to stay away from dissecting on the postero-superior neck/retinaculum where the nutrient arteries enter the head. That's another reason in my mind to stay away from a formal KL
3. I don't use flouro with the head dislocated, I can see into the joint, the entire femoral head/neck. Ijust check a plain film at the end for screw legnth.
IF pelvis is stable..Do you have to fix the SI? I'm not sure its going to help the patient.
Thanks
Brian
Date: Wed, 17 Nov 2004 08:40:35 -0800
From: Chip Routt
Thanks.
With your surgical dislocation and the patient positioned laterally, how do you maintain the neck fracture reduction as you insert the screws?
I was unaware that a KL exposure included a capsular dissection at the postero-superior neck.
His pelvis examines stable to palpation but the SI joint-iliac fracture is displaced according to the images.
Chip
Date: Thu, 18 Nov 2004 13:07:28 -0800
From: Chip Routt
Maybe we should all review and reread again the articles that Brian references.
When I reread them, I was unable to find any "dual approaches" discussed in Marchetti's (J Orthop Trauma. 1996;10(7):455-61) paper... not one.
Swiontkowski's paper (J Orthop Trauma. 1992;6(4):437-42) reports their results focused on Pipkin I and II type fractures only. They do mention that they had 5 of their 41 total patients with type IV injuries, and only 2 of those 5 were treated with "combined simultaneous anterior and posterior approaches" ... but no results are provided for those 2 patients with type IV injuries ... unless I misread/misunderstood the articles, or totally missed the data point.
Chip
Date: Wed, 17 Nov 2004 09:32:59 -0600
From: Sam Agnew, M.D.
Chip
Good morning, and thanks for an interesting mid-term exam, as the n pertaining to this injury compilation should generate a nice discussion.
Before I commit to a tactic, some questions regarding the injury and the patient:
Is he obese (meso-ecto-endomorph?)
Does he have any significant degloving injury to go along with that vehicular mechanism?
I cannot ascertain where the pelvic ring exits-by your exam it was stable (Y) and the injury is completely contained within the ipsilateral hemipelvis? His head fracture appears to be biplanar-crush injury (Y/N)? vs a single plane cleavage fracture
thanks, I will devise a tactic asap
Sam Agnew, MD, FACS
Orthopaedic Trauma
Date: Wed, 17 Nov 2004 08:51:40 -0800
From: Chip Routt
Hi Sam, thanks.
His exam and the CT images show that his body habitus is quite thin and well muscled, and without obvious soft tissue degloving injuries.
The pelvic mechanical exam was without obvious instability.
The anterior femoral head fragment is large and involves the fovea area but not above...it also has a thick cancellous foundation...and is a single planar fracture surface without comminution...it's a dream!!...it has 2 mm of frail residual stretched periosteal attachment at it's caudal-most edge.
The extruded head-neck fragment has local chondral abrasions and a focal area of impaction on the head...it still has posterior-superior soft tissue attachments.
The neck fracture is horizontal and somewhat comminuted, but not too bad.
The ligamentum teres remains anchored to the fossa acetabuli but has been torn away from the extruded head-neck fragment.
Chip
Date: Wed, 17 Nov 2004 13:02:57 -0600
From: Sam Agnew, M.D.
His exam and the CT images show that his body habitus is quite thin(like his surgeon) and well muscled (ditto), and without obvious soft tissue degloving injuries.(very lucky) ...
I would chime in with:
Supine on a completely radiolucent table
Femoral distractor from ilium to femur for intraop traction as needed for neck length restoration
C-arm from contralateral side with visualization of head-neck confirmed at initiation
Smith Peterson approach with ORIF-direct of head-&-head neck component with medial neck buttress plate (maxillofacial or mini fragment) with bone graft if needed ( I find that it often is) screw fixation of head component. Femoral distractor to restore Head-neck alignment-length as needed for reduction.
Adjunctive Neck-proximal shaft fixation with short barrel-short side plate compression screw, if adequate window following head-neck component plating-pediatric compression plate if diameter window an issue or my preference in most segmental neck injuries-- position screw stabilization along tension and compression trabecular planes.
Supine- ilio-sacral screw reduction-stabilization of the SI joint (per Letournel preaching-ipsilateral SI-Acetabular fractures)
Femoral distractor from Medius to medius pillar if reduction to SI needed-and a further eval of contra SI
Prone Kocher to address the posterior wall- posterior dislocation fragment-component-debride minimus as indicated by amount of contusion-dysvascularity to mass, retain inf. gemelli attachment if feasible.
But then again I could be wrong
sga
Date: Wed, 17 Nov 2004 11:11:41 -0500
From: James Carr
Chip
I have fixed some similar ones. In the few I have done, disastrous AVN occurred. I would concur more with Adam's approach. The posterior wall fracture is large enough to get exposure to the head, and allows a more extensile troch osteotomy as mentioned. I would feel more secure with a screw/2 hole side plate if it is a vertical pattern.
Imaging in the lateral decubitus is simple. The key to getting a good lateral hip view is to make sure the bottom hip is extended, and the patient can be leaned forward slightly. One then brings the C-arm in with the "C" tilted towards cephlad, and "over the top" slightly. This will get an awesome lateral. (Hope I explained it so you can visualize it).
With regards to the femoral head, I would think it is fixable through the posterior approach. My preferred approach to the head fx in isolated circumstances is the medial approach, which is a bloodless internervous plane, and doesn't affect blood supply to the head. It also allows direct placement of the screws perpendicular to the fracture surface.
I have done the vertical posterior incision S-I approach, and the K-L at the same time, and only did it once. I polished some stainless steel screw heads for a few months for that great idea. However, a perc screw is just fine. Any problem with reduction of the S-I, and I would go anterior in a supine position.
Jim Carr
James B. Carr, MD
Premier Orthopedic Specialists
Columbia, SC 29203
Date: Wed, 17 Nov 2004 08:34:21 -0800
From: Chip Routt
Thanks.
His neck fracture is horizontal.
Can you describe the details of your similar patients...did they have extruded head-neck fragments too?
Did any of them avoid AVN?
If not, would you continue to fix them knowing that they are going to get AVN?
Thanks-
Chip
Date: Wed, 17 Nov 2004 12:50:45 -0500
From: James Carr
The similar patients had Pipkin IV without extruded piece + femoral neck (2) ; one had femoral neck fracture that spilt the acetabulum in half, and the head wound up in the pelvis. All 3 had AVN, and 2/3 required hemiarthroplasty. I think it is definitely worth a try since he is 22. When I was a fellow Steve had one where there was a segmental femur/ femoral neck/posterior wall and dislocated femoral head. We did her prone, and cut off a rod to do a retrograde nail after we screwed the neck and fixed the acetabulum. From my understanding, the head lived, but she did need a procedure for her distal femoral nonunion.
Date: Tue, 16 Nov 2004 17:53:55 -0800
From: Chip Routt
We initially did an ORIF of the femoral neck and then the head using a modified Smith-Petersen exposure with the patient positioned supine. The femoral head fracture fragment was without soft tissue attachments and removed temporarily. The ligamentum teres had been disrupted from its femoral head attachment so it was debrided. The dislocated head-neck fragment was then rotated out of the posterior impaction area, manipulated into the acetabulum preserving it s limited capsular remnants, rotated it to fit the neck, and then stabilized with screws inserted through stab wounds and guided by fluoroscopy. Then we reduced and used small screws to hold the previously removed femoral head fracture fragment.
For a variety of reasons we stopped at that, placed him in traction, and repeated his films and CT.
Two days later we returned to the OR and tried a closed manipulative reduction of the SI joint-iliac fracture but it failed, so we used the lateral (iliac) window of an ilioinguinal exposure to clean, reduce, and clamp the SI joint. We stabilized it with an iliosacral screw and closed.
Under the same anesthesia, we used a prone K-L exposure to reduce the impaction fragment, fold down the posterior wall, and hold it with a plate.
Here are the films....the staple lines mark his incisions.
 |
 |
 |
We'll use ectopic bone prophylaxis and protect his weight bearing.
Several of us are curious if anyone's ever seen such an injury result in a viable durable femoral head?
Any other ideas?
Thank you-
Chip
Date: Fri, 19 Nov 2004 11:38:43 -0500
From: James Carr
Looks super Chip - very nice technical execution
Jim
James B. Carr, MD
Premier Orthopedic Specialists
Columbia, SC 29203