

Date: Tue, 2 Jul 2002 00:49:20 +0530
Subject: Fracture femur with pelvic disruption
I am presenting this case for opinion of list members.
Middle aged male who was injured when a log of wood fell on him ina saw mill. Haemodynamically patient stable. No visceral injuries detected. The following musculoskeletal injuries detected: 1) Closed fracture femur. 2) Pubic symphysis disruption. 3) Right inf pubic rami fracture. 4) Right acetabular fracture. Head of femur located. 5) Right Sacroiliac joint anterior opening.
I plan to do the following: 1) Closed interlocking nailing of femur in the lateral position without perineal post(Have done a few in this position and am quite happy about it.) 2) External fixation of pelvis with schanz screws on either anterior iliac crest to apply compresion to iliac wings. 3) Open reduction and plating of pubic symphysis. I will be happy to know the opinion of the list members on the case and my management plan.
 |
 |
 |
 |
 |
 |
 |
 |
Dr.T.I. George, Consultant Orthopaedic Surgeon,
Polytrauma, Microvascular Surgery And Hand Surgery Unit,
Metropolitan Hospital, Trichur, S.India.
Date: Mon, 01 Jul 2002 15:05:50 -0500
From: Adam Starr
Dr George,
Your plan sounds fine. The acetabular fracture looks like a high ramus fracture that happens to enter the acetabulum. The CT scan is blurry, and you haven't provided any oblique views of the acetabulum - but my guess is that the 'tab is concentric.
Kyle Dickson and Joel Matta published a series of anterior ring injuries - mostly rami fractures, if I remember right - and they concluded that you could ignore most of them. I think Kyle says you should operate if they're displaced more than 2 cm or so.
At any rate, I think the experts would recommend non-operative management of the ramus fractures.
I would treat the femur with an IM nail, as you plan to do. The ex-fix frame can be used as a reduction tool to allow easy plating of the symphysis. OR, you could just use a clamp to hold the reduction while you do the open symphyseal plating.
I think the anterior opening of the SI joint will close down once you repair the symphysis diastasis.
Good luck,
Adam Starr
Dallas, Texas
Date: Tue, 02 Jul 2002 10:52:25 -0400
From: James Carr
Beware displacing the acetabulum with the plating. I would think the ex fix would close things nicely by itself.
JBC
Date: Wed, 03 Jul 2002 19:23:00 +0530
From: DR T I GEORGE
Dear List members,
Thank you very much for your various contributions on this case. At about 36 hours after presentation this case was taken up for surgery and by this time it was obvious that there were no visceral catastrophies that were hidden. Patient who was a chronic smoker started running a low grade fever and a cough with yellowish sputum at this time. Antibiotic cover was given adequately. The lab values just before the surgery showed a rise in CPK to the tune of about 1200 units and all other haematological and biochemical parameters were well within normal limits. Closed nailing of femur and external fixation of pelvis with closed reduction of pubic symphysis were done to get an acceptable position. Immediate post op time the thigh was swollen but not tense. Lab values soon showed another 1000 units rise in CPK and urine was quite dark. Our nephrology colleague started to alkalinise the sytem by giving sodabicarb IV. In a couple of hours the thigh became quite tense and an emergency fasciotomy was carried out in the ICU. The next 12 hours showed an increase in CPK by about 5000 units thus taking it well above 7000 units. Having got an established Rhabdomyolysis, Diuretics were started along with alkalinising. Nephrology colleague warned us on the fluid which has gone to third space coming back as the Rhabdomyolysis settles down. Sure enough as the CPK started to come down pulmonary function started to deteriorate. Patient had to be put on ventillator about 48 hours after surgery was over. To day his lungs are better and weaning process has started.
Here are the post op pictures.
 |
 |
I would welcome comments and criticisms. I have a couple of questions to the list: i) How often do you see Rhabdomyolysis (Old term - crush syndrome) ? We have been seeing it on and off. ii) One of the list members suggested using fracture table and traction. I did the femur in lateral positon without traction. How safe is it to use fracture table with perineal post in the presence of pubic symphysis diastasis?
Dr.T.I. George, Consultant Orthopaedic Surgeon,
Polytrauma, Microvascular Surgery And Hand Surgery Unit,
Metropolitan Hospital, Trichur, S.India.
Date: Fri, 12 Jul 2002 23:50:58 +0530
From: DR T I GEORGE
I am posting this question separately since I did not get responses when I posted these along with the case which I had posted recently. How often do list members see Rhabdomyolysis - myoglobunuria - leading to renal dysfunction and pulmonary function after trauma? What is the protocol for managing the same in different centres?
Dr.T.I. George, Consultant Orthopaedic Surgeon,
Polytrauma, Microvascular Surgery And Hand Surgery Unit,
Metropolitan Hospital, Trichur, S.India.
Date: Fri, 12 Jul 2002 14:13:59 -0500
From: Steven Rabin
I have seen it 4 or 5 times in the past 10 years where it was full-blown rhabodomyolysis (as opposed to more frequent myoglobinuria). In all of these patients, they were big muscular guys with femur fractures where we did antegrade nailing and took a long time to do the case - (now similar patients benefit from the retrograde approach) ... 2 of these patients had documented cocaine use, which by itself is a risk factor for rhabdomyolysis, and 2 had prolonged extraction times, which is also a risk factor.
Treatment is supportive. Compartment fasciotomies are useful early. Debridement of dead muscle is also necessary.
Date: Sun, 14 Jul 2002 8:30 AM EST
From: Bill Burman
An online reference for rhabdomyolysis may be found at:
http://www.emedicine.com/EMERG/topic508.htm
Bill Burman, MD
HWB Foundation
Date: Sun, 14 Jul 2002 10:47:00 -0400
From: Frykberg, Eric
This is an interesting case of apparent spontaneous crush syndrome s/p fracture fixation with full blown compartment syndrome being appropriately treated when found. The question that comes up is what premonitory signs or levels of suspicion may have been present or possible before this came to such an advanced clinical state? Finding compartment syndrome only after it has occurred with massive irreversible tissue damage should generally be seen as a diagnostic failure. In the presentation of the case, interestingly, no info is given as to the status of vascular perfusion, pulses, etc, but I will assume they were normal then. After compartment syndrome, there was still no info provided as far as evidence of vascular injury, so I will assume there was none, and there were no misssed vascular injuries here
That leaves the fracture alone as the underlying etiology--so, with such massive polytrauma fo orthopedic injuries, should not a prophylactic fasciotomy have been considered. This more aggresssive use of fasciotomy in complex extremity trauma has clearly been associated with improved limb salvage and function in the trauma literature--by aggressive, I mean performing it as early as possible, even prophylactically in hi-risk scenarios, with the goal of preventing rather than treating its onset. Even if not performing it prophylactically, a hi risk limb as these were should be monitored regularly--however, not by phys exam, whose pitfalls are clearly illustrated by this case--by waiting for obvious clinical manifestations, you are too late. Direct compartment pressure measurements should be serially monitored, with fasciotomy at the slightest increase, or any pressure over 20-25mm Hg.
Could these limbs not have been recognized at presentation and postop as posing a high enough risk for compartment syndrome to have allowed earlier intervention with the above options??
ERF
Date: Mon, 15 Jul 2002 00:22:11 +0530
From: DR T I GEORGE
I would like to respond to Frykberg, Eric's mail as follows:
" The question that comes up is what premonitory signs or levels of suspicion may have been present or possible before this came to such an advanced clinical state"
There was a high level of suspicion of this patient developing complications like ARDS and Rhabdomyolysis. That is the very reason we kept monitoring pulmonary function and CPK levels apart from regular clinical evaluation and other laboratory investigations. In fact pre to post op the CPK went up by about 1000 units. Immediate post op the thigh was swollen but not tense, but went tense in a few hours.
"In the presentation of the case, interestingly, no info is given as to the status of vascular perfusion, pulses, etc, but I will assume they were normal then. After compartment syndrome, there was still no info provided as far as evidence of vascular injury, so I will assume there was none, and there were no misssed vascular injuries here "
There were no neurovascular deficit pre or post op period.
"Even if not performing it prophylactically, a hi risk limb as these were should be monitored regularly--however, not by phys exam, whose pitfalls are clearly illustrated by this case--by waiting for obvious clinical manifestations, you are too late. Direct compartment pressure measurements should be serially monitored, with fasciotomy at the slightest increase, or any pressure over 20-25mm Hg."
This patient was regularly monitored as was presented to you. We still rely on clinical judgement a lot and do not entirely go by lab values or other readings from gadgets in managing a patient. The supportive evidence >from equipments are valuable but clinical evidence has to corraborate readings. From the practical point of view of compartment pressure readings, I am not aware of any gadgets freely available for us in this country which is reliable.
"Could these limbs not have been recognized at presentation and postop as posing a high enough risk for compartment syndrome to have allowed earlier intervention with the above options?? "
Yes it was recognised from presentation, closely monitored and appropriate action was taken as and when necessary.
Dr.T.I. George, Consultant Orthopaedic Surgeon,
Polytrauma, Microvascular Surgery And Hand Surgery Unit,
Metropolitan Hospital, Trichur, S.India.
From: Frykberg, Eric
Date: Sun, 14 Jul 2002 17:17:08 -0400
In reply--
In fact, both CPK levels and "clinical evidence"--i.e. physical findings, are well known and well documented in the literature to be notoriously insensitive and unreliable at detecting compartment syndrome when it needs to be found -- BEFORE the development of full blown crush syndrome. If this case does not fully illustrate this point, then nothing will. Measurement of compartment pressures, if not prophylactic early fasciotomy, is widely published as how best to avert a case such as this. If as you say you had the suspicion for this beforehand, the answer to your original question for thoughts on the management or anything else that may have been considered, is as I mentioned -- earlier attention to fasciotomy before the development of "clinical evidence". I will be glad to post citations for this if you like, but most of them come from the Orthopedic literature -- these principles have been in this literature for over 20 years.
ERF
Date: Sun, 14 Jul 2002 18:59:03 -0400
From: Ernest Block, MD
CPK levels
We know that from the "old days" when many centers measured CPKs for "cardiac contusion" that almost every trauma patient has a rise in CPKs. Prevent rhabdo when you can, when not, stick with volume resuscitation as therapy.
As always, physicians feel the need to measure SOMETHING even if it has no proven value, obvious pain for the patient and added cost.
Date: Sun, 14 Jul 2002 22:20 EST
From: Bill Burman
From the practical point of view of compartment pressure readings, I am not aware of any gadgets freely available for us in this countrywhich is reliable.
In a classic OTA Basic Fracture Course Lecture, Thomas Whitesides shows a relatively simple and inexpensive system for compartment monitoring which he claims is reliable.
Bill Burman, MD
HWB Foundation
Date: Tue, 16 Jul 2002 19:18:15 +0530
From: DR T I GEORGE
FE: "I will be glad to post citations for this if you like, but most of them come from the Orthopedic literature".
Iwill be thankful for the same. i will be travelling for a few days and may not be able to check my mail for a couple of days from tomorrow. Bur will do it at the earliest.
Dr.T.I. George, Consultant Orthopaedic Surgeon,
Polytrauma, Microvascular Surgery And Hand Surgery Unit,
Metropolitan Hospital, Trichur, S.India.
Date: Tue, 16 Jul 2002 16:06:09 -0400
From: Frykberg, Eric
Frykberg ER: Compartment Syndrome, in Current Surgical Therapy, Cameron JD (ed) 5th edition, /WB Saunders, Philadelphia, 1995, pp. 850-855.
Mubarak SJ, Owen CA: Double-incision fasciotomy of the leg for decompression in compartment syndromes. J Bone Joint Surg 1977;59A:184-187.
Vitale GC, Richardson JD, George SM, et al: Fasciotomy for severe, blunt and penetrating trauma of the extremity. Surg Gynecol Obstet 1988;166:397-401.
Sheridan GW, Matsen FA: Fasciotomy in the treatment of acute compartment syndrome. J Bone Joint Surg 1976;58:112-115.
Attebery LR, Dennis JW, et al: Changing patterns of arterial injuries associated with fractures and dislocations. J Am Coll Surg 1996;183:377-383.
Feliciano DV, Cruse PA, Spjut-Patrinely V, et al: Fasciotomy after trauma to the extremities. Am J Surg 1988;156:533.
McDermott AGP, Marble AE, Yabsley RH, et al: Monitoring acute compartment pressures with the STIC catheter. Clin Orthoped 1984;190:192.
Mubarak SJ, Hargens AR: Acute compartment syndromes. Surg Clin North Am 1983;63:539.
Williams AB, Luchette FA, et al: The effect of early vs. late fasciotomy in the management of extremity trauma. Surgery 1997;122:861.
ERF
Date: Tue, 16 Jul 2002 19:20:59 +0530
From: DR T I GEORGE
MayI pose this question to the list. Is it safe to use fracture table with traction against a perineal post in the presence of pubic symphysis diastasis?
Dr.T.I. George, Consultant Orthopaedic Surgeon,
Polytrauma, Microvascular Surgery And Hand Surgery Unit,
Metropolitan Hospital, Trichur, S.India.
Date: Tue, 16 Jul 2002 20:20:17 EDT
From: Aobonedoc
Have never seen this but I would think you could. Be gentle on the traction.
M. Bryan Neal, MD
Date: Wed, 17 Jul 2002 07:58:48 -0700
From: Chip Routt
Is it safe to use fracture table with traction against a perineal post in the presence of pubic symphysis diastasis?
The answer would depend on numerous patient- and fracture-specific factors/details.
How about this, reduce and stablize the symphysis (and posterior ring) injury(ies) initially, then fix the femur without a traction table.
Chip
M.L. Chip Routt, Jr.,M.D.
Professor-Orthopedic Surgery
Harborview Medical Center
Seattle, WA 98104-2499
Date: Wed, 17 Jul 2002 11:00 EST
From: Bill Burman
Is it safe to use fracture table with traction against a perineal post in the presence of pubic symphysis diastasis?
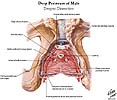
The pelvic injury appears to be an APC1 (AP Compression) by the Young-Burgess classification.
Dalal, Young, Burgess and Siegal report a 9% incidence of GU injury with APC1.
Further pelvic AP compression by driving a fracture table perineal post against an injured perineum with possible urethral, bladder, rectal and/or pudendal nerve attenuation sounds risky.
 |
Date: Tue, 1 Oct 2002 21:58:16 +0530
From: DR T I GEORGE
Friends I would like to give the follow up of this case which I had presented in early July 2002.
To recap: Middle aged male patient on whom a heavy log fell and sustained injury. Had pelvic ring disruption with fracture femur. Ext fix of pelvis and interlocking nailing of femur done. Developed compartment syndrome thigh and had fasciotomy. Went on to rhabdomyolysis and ARDS. Managed with ventillation and alkalinising. Fasciotomy wound later skin grafted.
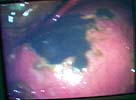
Now what I have not told so far: At about three weeks after the injury when patient had recovered from the problems described above developed acalculous cholecystitis. As he was being prepared for surgery he suddenely collapsed and went into shock. Required resuscitation and inotropic support. After vital signs were stable he was taken up for laparoscopic cholecystectomy. On introducing the scope it was found that there was a gangrenous gall bladder with lots of inflammation all around. It was converted to an open cholecystectomy. Ventillated post op. Patient's ext fix on pelvis was removed after six weeks and ambulated with walker. Had developed a deep sacral pressure sore. Discharged with home care of pressure sore and ambulation with support. Now at about three weeks the femur is uniting, pelvis stable and the pressure sore healing. Patient changed to axillary crutches from walker.
My question to the list: How often do you see acalculous cholecystitis following pelvic fracture? Any other comments?? Laparoscopic picture of gall bladder and present x-rays attached.
 |
 |
 |
Dr.T.I. George, Consultant Orthopaedic Surgeon,
Polytrauma, Microvascular Surgery And Hand Surgery Unit,
Metropolitan Hospital, Trichur, S.India.
Date: Tue, 1 Oct 2002 11:52:56 -0500
From: Adam Starr In my experience, acalculous cholecystitis is usually seen in sick sick
patients who've spent a lot of time in the ICU.
Seems to me that the ones who get it are the ones who've been septic on
and off, and hypotensive, and who've been starved (or not able to eat
because of the ventiliator or whatever). I guess not eating screws up
your biliary system somehow.
I don't think the pelvic ring injury really has much to do with it,
except as a marker of severe injury.
I think taking the galbladder out is the right thing to do. Not
surprising that you had to convert to open cholecysectomy - I think the
bladder wall gets fibrotic and scarred down when they get this disease.
But, I'm no general surgeon. Maybe one of the folks from the AAST list
can weigh in with some smart comments.
Adam Starr
Date: Tue, 1 Oct 2002 23:59:39 +0530
From: DR T I GEORGE
Thanks Adam. I am also not a General Surgeon. That part of the job was done
my colleague Dr Jayachandran.
Dr.T.I. George, Consultant Orthopaedic Surgeon,
Date: Tue, 1 Oct 2002 22:21:02 +0200
From: Victor de Ridder
In my experience as general surgeon/traumatologist with ICU license, we see
such patients rarely, but only in the very sick patients with multiple organ
system failure or multiple trauma, as in the presented case. Literature tells us
: 3-5 % of such cases, so in a big trauma center probably once per year. No
specific relation with the pelvic ring fracture, just in relation to the multiple
organ disease. And then the gallblader looks exactly like the pictures you
presented: the ongoing infection causes ischaemia and necrosis.
Hope this helps, greetings from The Netherlands,
Victor de Ridder.
Dallas, Texas
Polytrauma, Microvascular Surgery And Hand Surgery Unit,
Metropolitan Hospital, Trichur, S.India.