



Date: Tue, 1 Jul 2003 23:10:54 EDT
Subject: Pelvic Fx with GU Injury
I'm looking for advice in managing pelvic fractures with coexistent GU injuries. I haven't been able to find a lot of literature on the subject besides Dr. Routt's article in CORR.
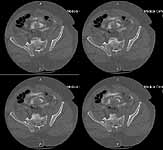
The patient is a 63 yo man who was crushed at work 5 days ago and sustained an unstable pelvic fracture with a GU disruption. I have assumed his care today. I am told he has an extraperitoneal bladder rupture but based on the cysto I am concerned about a urethral disruption. He does not otherwise have any significant injuries or medical problems, but he is severely obese (350 lbs+). Xrays and CT cuts are enclosed.
My plan: I would like to plate his symphysis in coordination with GU (who will repair his bladder at the same time) and ORIF vs CRIF his L SI joint and CRIF his R SI joint. My main concern is that he has a SPT (placed percutaneously on the day of admission in the ER with U/S) which is basically at the level of my Pfannenstiel approach and probably can't be draped out. His labs are okay and I am getting repeat labs tomorrow including U/A and C/S. Would anybody due anything differently? Do people think I'll be able to CRIF his SI joint after fixing him in front? Use the C Clamp or just use the SI screws to squeeze (I've done that before--as late as 2 weeks--successfully)?
 |
 |
 |
 |
 |
 |
 |
If people think this is a reasonable plan, what would people do if his UA were positive or if the SPT had been in for 2 weeks? Any tips on avoiding these situations?
Thanks for your advice,
Peter Krause, MD
LSU.
Date: Tue, 1 Jul 2003 22:52:07 -0500
From: Andrew H. Schmidt
This is always a potential dilemma best avoided by finding and nourishing a relationship with a urologist who is interested and willing to help. At our center, I haven t seen a suprapubic catheter used for ages. With bladder ruptures, we do just what you suggest place a Foley for drainage and Urology repairs it at the time of symphysis plating. With urethral injuries, we go ahead and pass a Foley, and if there are problems Urology comes in and gets it in for us. With either situation, the Foley is left in place for a longer period of time, with the duration depending on the nature of the urogenital injury.
When a patient is transferred with a suprapubic catheter in place, we try to get Urology to deal with it and get it out ASAP, and if we can t we treat the case like an open fracture at the time of fixation with copious irrigation and sometimes a second irrigation.
Regarding your case, at our center he would get a symphysis plating, bladder repair, and hopefully urology could remove the SPT and get a Foley catheter in place. Then we would do an open reduction of the left Si joint though the posterior approach (prone position) with iliosacral fixation using 2 lag screws.
Andy Schmidt
Date: Wed, 2 Jul 2003 08:50:55 -0500
From: Kyle Dickson, MD
Hey peter, difficult problem. This far out I think it s hard to reduce from the front first. I would start posterior get both sides reduced (orif) and fixed with iliosacral screws then turn the patient over and pull the suprapubic and treat like and open wound with i&d followed by reprep and draping. Then do an orif of the symphysis. At that time the urologist can place a foley or tunnel a suprapubic catheter (should be done initially so you can prep it out of the wound without contamination). Hopefully this helps if you have any questions give me a call.
kyle
From: Krausepc
Date: Sat, 13 Sep 2003 02:25:06 EDT
Just a follow-up on a case I posted to the list earlier this year. Thanks to everybody who gave me advice. The original case: a63 yo man who was crushed at work 5 days ago and sustained an unstable pelvic fracture with a urethral disruption.Hehad been treated initially with a suprapubictube placed percutaneously in the ER. Did not otherwise have any significant injuries or medical problems, but was severely obese (about 450 lbs). The problem was that he had a suprapubic tube directly in line with a standard Pfannenstiel approach and the question was how to manage this.
What we did: I took him to the OR on hospital day 6 to fix his pelvis with the plan to remove the SP tube and place a foley. Because of his size and pelvic fracture I had requested an IVC filter preop but this could not be done in IR because of weight. The plan was to do this in the OR as well. In the OR his suprapubic tube was removed, but then while positioning him he had an apparent PE and coded. He was resuscitated and IR came in to put in the filter. No angiogram was done because of his very high pulmonary artery pressures. Urology did a cysto and found a partial urethral tear and they were able to pass a foley over a wire. We postponed the pelvic fixation in favor of continued resuscitation/stabilization.
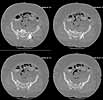
Five dayslater we was doing much better and was deemed fit for surgery. The site of his SP tube had completely healed up without evidence of infection. We took him to the OR to plate his symphysis, making our Pfannenstiel incision low to avoid the SP site. During plating we notice at one point some murky fluid in a little pocket deep inside his pelvis. The was sent for gram stain and culture and came back GPC and ultimately grew out enterococcus. We completed the symphseal plating & packed the wound with antibiotic beads. We brought him back at 48 hours for repeat I&D and removal of the beads and closure. He tolerated both of these surgeries well. About 5 days later(roughly 2 1/2weeks afterhis injury)his wound in the front was looking good and there was no evidence for infection. So he was brought back to the OR for posterior pelvic fixation. My plan had been to do an ORIF and place SI screws, but I couldn't get adequate inlet or lateral views. So we did an open reduction and posterior transiliac plating. The reductions in the front and the backwere difficult due to both his size and due to the time that had elapsed since his injury.I've enclosed pre and post xrays.
 |
 |
 |
 |
 |
He has done extremely well postoperatively and infection has not recurred. This case has raised one further question, which our trauma committee is actively considering: which patients should receive prophylactic IVC filters?What are listmembers doing in their hospitals?
Sincerely,
Peter Krause, MD
LSU Department of Orthopaedic Surgery