Subject: Sacral Fracture
Date: Fri, 7 Mar 2003 21:08:10 -0600
Hi,
40 yr old fit and healthy manual worker fell down from a 10 ft electric pole and was brought in with no BP and slow pulse. suspicion of electrocution was there due to the bradycardia which could also be due to being good fitness as well. was conscious though. revived well with IV fluids etc. Xrays show a suspicion to the left of the sacral body, through the sacral foramina which was confirmed on later CT. USS abdo was normal. Xrays also show a fracture thhrough the antr wall of the left acetabulum, basically at the junction of the supr pubic ramus with the acetabulum, and also fractures of both infr pubic rami, and a fracture through the right supr pubic ramus just medial to the acetabulum. So, he has a vertical shear/vertically unstable left hemipelvis fracture. Initial stabilisation with an antr iliac wing exfix has been done and screening shows very minimal mobility at the sacral level.
My question is, should we fix the left antr wall fracture through an ilio-inguinal approach and also the postr sacral fracture with either canc ilio-sacral screws and avoid prolonged exfix?? or is exfix also necessary anyway even after front and back fixation? or is exfix alone enough?
does anyone use the 2 sacral bars/rods still nowadays? or have you all shifted to the sacral body canc lag screw method for unstable pelvic fractures inv. the sacrum through the sacral foramina or lateral to it?
also has anyone done this with the patient in the lateral position? I know it is usual to do this in the prone position, but I have a patient in whom an ext fixator has been applied as an emergency procedure who will benefit from a sacral canc screw or rod as well. The question is how to put in the screws now with the fixator in place antrly. He has left antr wall acetabular fractures, which are being treated conservatively(stable on screening), and an unstable vertical shear fracture of the left hemipelvis which is being held reasonably with the antr pelvic fixator.
with warm regards
girish kumar
Date: Fri, 7 Mar 2003 19:51:33 -0800
From: Chip Routt
The supine position allows routine iliosacral screw insertion if the patient is elevated on a lumbosacral support, usually 1-2 folded blanket(s). The frame can be used as a manipulative reduction device intra-operatively. Supine positioning allows numerous treatment options.
Browner described using two OR tables end-to-end if the prone position is necessary...the anterior pelvic ext fix hangs between the two table ends...I've never tried it.
Lateral positioning denies almost all pelvic reduction maneuvers and complicates routine imaging.
Supine is our choice, unless we need a posterior exposure for open reduction.
Chip
M.L. Chip Routt, Jr.,M.D.
Professor-Orthopedic Surgery
Harborview Medical Center
Seattle, WA 98104-2499
Date: Sat, 8 Mar 2003 04:39:51 -0500
From: nvgirish
Thanks very much. have not come across supine iliosacral screw fixation before. this will be ideal as prone positioning in such severe injuries is not appealing to me at all. Please tell me how difficult it is to do it in supine psoition. How much angling of the C arm do you have to do to see the sacral body antrly??
please let me know any more thoughts on this matter. would you fix the left acetabulum?
rgds
girish
Date: Sat, 8 Mar 2003 07:11:26 -0800
From: Chip Routt
It would be good to see the plain films and a few more sacral axial images if possible.
Chip
M.L. Chip Routt, Jr.,M.D.
Professor-Orthopedic Surgery
Harborview Medical Center
Seattle, WA 98104-2499
Date: Sat, 8 Mar 2003 09:30:07 -0600
From: Sciadini, Marcus
Supine positioning for placement of iliosacral screws is not significantly more difficult than prone, and is for many surgeons the position of choice. The degree to which the C-arm is angled for your inlet and outlet views is really no different, when you think about it...only the reverse orientation! The midline bump is key as it elevates the sacrum up to an accessible level, using blankets instead of sheets minimizes the flouroscopic artifact produced by the bump and as always, confirming your ability to obtain adequate inlet and outlet views and visualize the foramen and anterior/posterior extent of the sacral body is important prior to the sterile prep and drape. A true lateral of the sacrum with your c-arm gives you a good starting point for your incision.
Marcus F. Sciadini, M.D.
Assistant Professor, Dept. of Orthopaedics & Rehabilitation
Vanderbilt University School of Medicine
Nashville, TN
Date: Sat, 8 Mar 2003 07:53:19 -0800
From: Chip Routt
It's no more difficult supine than it is prone, as long as you elevate the patient's pelvic region from the operating table on a lumbosacral support. There is no difference in degree of difficulty.
Many surgeons prefer prone positioning because they believe that open reduction is necessary using a posterior exposure. Some also use posterior iliac osseus landmarks to help them understand the drill/screw starting point, etc. If you rely on these variable bony landmarks, then you can't do them supine.
If you understand the anatomy, injury, and intra-operative correlative imaging, then "supine screws" will be good for you and your patient when indicated.
Supine positioning concerns some surgeons because the posterior ilium is adjacent to the table. For your initial supine iliosacral screws, simply position/move the patient closer to the table edge...but make sure that you won't need a contralateral screw!!
Traction can be maintained using prone or supine.
The intra-operative imaging is routine/uncomplicated with the patient positioned supine or prone.
As you know, the amount of "angling of the C arm" is unique to each patient depending on their lumbosacral lordosis, presence of lumbosacral transitional vertebra, patient positioning, and specific injury pattern... usually it's between 30-50 degrees of approximate "angling" for the pelvic inlet image. We adjust the image tilt until the upper sacral vertebral bodies are superimposed. The lateral sacral image confirms it.
For the outlet intra-operative fluoroscopic image, we'd recommend positioning the beam so that the top of the symphysis pubis area is superimposed on the second sacral vertebral body...also between 30-50 degrees...biplanar views.
Lateral sacral imaging is the same for supine and prone.
Don't forget - accurate imaging relies on accurate reduction.
If you have malreduction, the doctor's understanding of the imaging is complicated.
If you have poor imaging, then fluoroscopic assessment of either open or closed reduction is impaired.
Malreduction challenges safe screw insertion.
The acetabular fracture involvement is termed a "pubic root fracture" in our institution and others. True, the anterior acetabular wall region is involved in this fracture, but it's not a true "anterior wall" acetabular fracture, which would imply anterior fracture-dislocation of the hip. The anterior wall area itself is quite small, and the true "anterior wall acetabular fracture" is an unusual fracture pattern.
Conversely, comminuted pubic root fractures involving the anterior acetabular wall and low anterior column areas are extremely common. They can be stabilized using the external frame, a medullary ramus screw, plate, (or combinations) as needed. We reserve formal ORIF of these injuries for those that involve the acetabular weight bearing area rather than the low anterior wall/column areas.
Thanks-
Chip
M.L. Chip Routt, Jr.,M.D.
Professor-Orthopedic Surgery
Harborview Medical Center
Seattle, WA 98104-2499
Date: Sat, 8 Mar 2003 11:37:57 -0600
From: girish kumar
In response to: Marcus F. Sciadini, M.D.
how big an incision do you make? is it possible to do this percutaneously? if using 2 iliosacral screws and 1 medullary ramus screw, will an ex-fix be necessary and for how long in this case?? what do you mean - blankets instead of sheets??
Regards,
girish
Date: Sat, 8 Mar 2003 11:37:55 -0600
From: girish kumar
In response to: M.L. Chip Routt, Jr.,M.D.
thnx for superb comments and suggestions. hope you don't mind all the questions from me. you are a great teacher. will send more sacral CT cuts tomorrow.
pl look at the comments and queries below some parts of your reply.
>It's no more difficult supine than it is prone, as long as you elevate the patient's pelvic region from the operating table on a lumbosacral support.
what does that mean - like a thin long padded ruler so that the spine is elevated?? how high & thick do you need it to be? also do you use a very long drill bit? I am sure you only use 6.5 or 7 mm cannulated screws with the prelim guide wire.
>adjacent to the table. For your initial supine iliosacral screws, simply position/move the patient closer to the table edge...
most of our tables have a metal bar along the edges, even a lot of the ones in the UK, except 1 long radiolucent leg extension, that I can remember. Do you have any different tables nowadays?
Traction can be maintained using prone or supine.
do you use the traction leg attachments or just manual pull after prepping the legs and including them in the sterile area??
>The acetabular fracture involvement is termed a "pubic root fracture" in our institution and others.
I like that term, great way to describe it.
>be stabilized using the external frame, a medullary ramus screw, plate, (or >combinations) as needed. We reserve formal ORIF of these injuries for those
have seen that screw described in Ganz's osteotomy fixation. will 1 such screw be enough in a fracture like this? I know you cannot put more than 1 screw in that area. how long will the screw be usually?? also putting it in percutaaneously from the lateral wall of the ilium must be quite challenging - any tips on this??
thnx
girish
Date: Sat, 8 Mar 2003 11:00:24 -0800
From: Chip Routt
>> CR: It's no more difficult supine than it is prone, as long as you elevate the patient's pelvic region from the operating table on a lumbosacral support.
> GK:what does that mean - like a thin long padded ruler so that the spine is elevated?? how high & thick do you need it to be? also do you use a very long drill bit? I am sure you only use 6.5 or 7 mm cannulated screws with the prelim guide wire.
We use a folded OR blanket or two...each usually folded to 4 inches thick(tall), 12 inches wide, and 2 feet length. We use AO 7.0mm cannulated screws, but we used to only have routine 6.5 cancellous screws before the 7.0s were made...they worked fine.
>> CR: adjacent to the table. For your initial supine iliosacral screws, simply position/move the patient closer to the table edge...but make sure that you
> GK: most of our tables have a metal bar along the edges, even a lot of the ones in the UK, except 1 long radiolucent leg extension, that I can remember. Do you have any different tables nowadays?
We use an OSI(Jackson) radiolucent OR table without the metal siderails...we used to not have it either.
>> CR:Traction can be maintained using prone or supine.
> GK: do you use the traction leg attachments or just manual pull after prepping the legs and including them in the sterile area??
If prone, the traction bow is padded from the thigh, and the flexed knee avoids pretibial pressure. If supine, we use an adjustable traction device created by our machine shop workers and OR nurse from a pipebender. Typically not included in the sterile field.
>> CR: The acetabular fracture involvement is termed a "pubic root fracture" in our institution and others.
> GK: I like that term, great way to describe it.
I agree.
>> CR: be stabilized using the external frame, a medullary ramus screw, plate, (or combinations) as needed.
> GK: have seen that screw described in Ganz's osteotomy fixation. will 1 such screw be enough in a fracture like this? I know you cannot put more than 1 screw in that area. how long will the screw be usually?? also putting it in percutaaneously from the lateral wall of the ilium must be quite challenging - any tips on this??
That's too much to write...there are published clinical and biomechanical manuscripts regarding this technique. It's not difficult if the fracture is reduced and the anatomy allows and the imaging is good...lots of details, tons of tips, but the technique isn't hard.
Maybe you can come visit some time?
Chip
M.L. Chip Routt, Jr.,M.D.
Professor-Orthopedic Surgery
Harborview Medical Center
Seattle, WA 98104-2499
Date: Sat, 8 Mar 2003 13:18:12 -0600
From: Sciadini, Marcus
With adequate c-arm images and accurate interpretation of them, the IS screws may be placed in true percutaneous fashion (ie: 2-3 cm), assuming your reduction is possible in closed fashion.
I would not think rami screws were necessary in this particular case (Chip?), thus you could leave your anterior fixator for 6-8 weeks.
The use of a blanket instead of sheets is due to the fact that you are trying to elevate the sacrum away from the bed. The blanket material is thicker than that of a sheet, so you can achieve more height with fewer folds in the material. Since each fold in the sheet or blanket is a potential air space, these often show up as flouroscopic artifact, obscuring your landmarks. Blankets are used instead of sheets to minimize the number of folds and thus minimize interference with your radiographic imaging.
One final point....try to make sure your anesthesiologists do not use nitrous oxide as an agent, as this tends cause an increase in bowel gas which can also cause problems with imaging!
Good luck!
Marcus F. Sciadini, M.D.
Date: Sat, 8 Mar 2003 3:37 PM EST
From: Bill Burman
A short while ago Dr. TI George also requested on-line sacral screw references pertaining to another unstable pelvic injury case:
http://www.hwbf.org/hwb/conf/georg19/pelsp.htm
On-line sacral screw references:
In case of a corpulent patient/GI/GU contrast/poor quality C-Arm, there was an interesting posterior pelvic ex-fix presented to the list a while ago.
http://www.hwbf.org/hwb/conf/shriv1/pelfx.htm
Date: Mon, 10 Mar 2003 02:25:39 -0500
From: nvgirish
Hi,
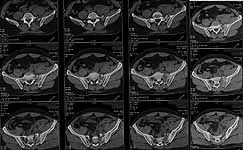
attaching the full CT cuts and 3D reformats which our radiologists love!
 |
 |
please let me know your thoughts.
am now convinced this is not a true vertical shear but a combined lateral compression with vertical shear type of injury. should use fully threaded lag screws for IS fixation. have only put in 2 schanz screws in the iliac wing. should I add medullary ramus screws or not? if so, can the screw be put in from the lateral iliac wing medially into the supr pubic ramus?? if putting in from the pubic symphysis, please describe the technique - how big an incision etc.
Date: Mon, 10 Mar 2003 06:08:33 -0600
From: girish kumar
hi,
>Maybe you can come visit some time?
thnx a million for the invite - would love to take it up some time later -
will be in touch when I come over next to the USA maybe next year.
this case and this list are just so educative and interesting for me and i
am sure others around the world that bill burman deserves a place in
e-heaven for maintaining it in such good nick. of course people like you,
Chip, Marcus & all the other regular contributors giving your experience
"freely" and voluntarily in the true and noble tradition that knowledge is
there to be passed on to all who want to update themselves is vital to this
endeavour too. you cannot imagine how useful it is to go through the
abstracts that bill burman has kindly given a list of - it is so difficult
to get copies of journal articles here or else so expensive(relatively
speaking in local currency) that I only wish people like you, Chip who have
written articles could put up your own work on the net for improving the
knowledge base in such parts of the world. Is that possible under the
copyright agreement that most journals get from authors?? India is highly
developed in lots of ways, but getting journal article copies is not 1 of
them unfortunately.
this case seems to be a vertically unstable sacral fracture with a
significant lateral compression injury too as seen on the axial CT's on
closer inspection. there is also no significant vertical translation, but
the left hemipelvis has definitley moved antrly in relation the the rest of
the sacrum and right hemiplevis. will every-one agree on this?? hence need
to be careful in not overtightening the IS screws and use fully threaded
screws if possible.
also please tell me how you put in the medullary ramus screw from the pubic
symphysis? i was thinking about putting it in from the other side, from the
lateral wall of the ilium, across the acetabulum into the supr pubic ramus.
would you it that way, at least in this case??
also on the topic of pelvic exfixes, do most people still use top of iliac
wing or have they shifted to AIIS area exfix site as a prefernce? i like
the AIIS area as it is much better bone and it is stronger and easier.
Regards,
girish
Date: Monday, 10 Mar 2003 9:02 AM EST
From: Bill Burman
Question: After review of the 2DCT and 3DCT images, is any internal or external pelvic fixation indicated?
Date: Mon, 10 Mar 2003 11:11:59 -0800
From: Chip Routt
Which method chosen is based on numerous patient factors-
Option #1
Option #2
The medullary ramus screw can be inserted in either direction, depending on
the details of the anatomy and injury.
He's had moderate-significant intrapelvic bleeding according to the 2D CT
images.
If we wait much longer, you'll be treating his DVT, PE, pneumonia, pressure
sores, etc.
Chip
M.L. Chip Routt, Jr.,M.D.
Date: Mon, 10 Mar 2003 11:54:13 -0800 From: Chip Routt > on the topic of pelvic exfixes, do most people still use top
of iliac wing or have they shifted to AIIS are a exfix site as a preference?
AIIS docking sites are popular these days for some surgeons (I don't
know why), but not for their patients...the soft tissue intervals are deep,
and the pins interfere with hip motion (sitting). We only use AIIS pin sites for those patients with fracture involving
the routine iliac crest sites...and temporarily for certain deformity corrections
using a distractor/compressor device on them. > please tell me how you put in the medullary ramus screw from
the pubic symphysis? i was thinking about putting it in from the other
side, from the lateral wall of the ilium Medullary ramus screws can be inserted with the patient supine or prone.
With the patient prone, they can only be inserted antegrade (from ilium
to pubis). We use a narrow diameter Kwire to arrive at the perfect starting
site and direction. The fluoroscopy views used are a pelvic inlet image
and a combination obturator oblique-pelvic outlet image. Take your time
positioning the Kwire perfectly, then tap it into the bone a bit before
incising the skin and deep soft tissues around it...one soft tissue tunnel
helps with screw insertion later, especially if it's a short length screw
in a fat patient. We use a long narrow diameter soft tissue protection sleeve/drill
guide to direct the drill and protect the tissues. Some like a cannulated
screw system. Try to make the glide hole perfect. The larger glide hole
drill in its sleeve is easier to manipulate...oscillate the drill if you
like. Use both views to stay extra-articular...on the inlet view as you
approach the joint, you will see the drill superimpose on the joint, but
remember it's above the joint on the other view, so it's OK. On the inlet
image, stay adjacent to the posterior endosteal cortex of the ramus. On
the obturator oblique-outlet combination image, stay above the dome aiming
for the mid-ramus medially. After you cross the fracture site, use the glide
hole drill to place a shallow "starting hole" in the medial fragment's
cancellous medullary bone...this helps the smaller diameter drill find it's
way into the correct medullary location. We use a calibrated narrow diameter
drill, and a soft tissue sleeve of known length to exact the drill depth
when we complete our drilling. Some like a cannulated screw system as mentioned.
Then insert the screw...the longer the screw, the easier to insert through
the soft tissue envelope. With a supine patient, the same is true for antegrade screws, but the
ipsilateral upper extremity and the OR table may get in your way, so anticipate
and make adjustments before you begin the procedure...no big deal if you
anticipate it. Retrograde (pubis to ilium) screws use the same images, but
with an oblique parasymphyseal soft tissue tunnel...spend some time with
pelvic models and then male and female cadaveric specimens to help you understand
the local anatomical potential frustrations and complications for each.
For both direction screws, patient positioning is important. Maybe do some medullary ramus screws initially in models and cadaveric
specimens using open, direct visualization techniques, along with the imaging
to stay safe and learn best...that is helpful for most. There are only about 500 other details. Safety first- Chip M.L. Chip Routt, Jr.,M.D.
Date: Thu, 20 Mar 2003 01:15:13 -0500
From: nvgirish
hi Prof Routt & all who helped in this case,
I am attaching the postop CT axial and coronal cuts with 2 iliosacral
screws in situ. I think there is probably 1 cm or so of upward movement at
the fracture site looking at it, but the II pics on table were not showing
it, so I decided to fix it in the same position without changing the exfix
alignment and just compressed the fracture site ever so slightly only. the
postop CT cuts were accomplished by our helpful radiologist who wanted the
images just as much as me, so we did it on "academic", no charge basis!
Happy to say the patient is well now, and relieved of pain. Am yet to
moblise him foot flat etc as advised by some, would prefer to wait for at
least 6 weeks in bed before doing so.
I would like to place on record the enormous gratitude and thanks from
myself and my patient for the superb guidance received from Prof Routt and
Dr Sciadini and Dr Burman, with online references on the supine ilio-sacral
screw technique that I performed with the help of this "on-line" CME. It is
ever so satisfying to me that this list has more than earned its place in
heaven with this 1 act of international Internet based co-operation. I
believe(correct me if I am wrong, Dr TI George, you may already have done
it this way) this is the first case done in India or at least in South
India to my knowledge in the supine position, with all the huge advantages
to the patient over the prone position. Of course, you need a very good C
arm and a competent radiographer to help in this, which I was fortunate to
have available in one of the good corporate hospitals in Coimbatore.
I would like to present this case to our local ortho societies and even a
forthcoming Asia Pacific Ortho Association meeting on Trauma being held in
Coimbatore with all your permission, as a method of helping advance the
treatment of patients all round the world.
warm regards
girish
Date: Thursday, 20 Mar 2003 10:33 AM EST
From: Bill Burman
Girish Thanks for the followup images. I think you make an important point regarding the quality of the C-Arm.
Perhaps the latter day corollary to the surgical dictum "Don't cut
where you can't see." should be "Don't drill where you can't C-Arm". My notes from
observing Joel Matta placing iliosacral screws in the prone position in
the mid 80's indicate an emphasis that the C-Arm needed to be at least 100
KV capable. While this sort of fluoroscopic capability is pretty much standard
in North America now, I would have concerns about widespread availability
abroad. Perhaps list members could comment on "minimum system (i.e. fluoro
and other) requirements" for iliosacral screws to accompany your anticipated
presentations. From: Matta, Joel M.D. Date: Sat, 29 Mar 2003 09:47:01 -0800 Bill Thanks for the request for the opinion. Overall I think it is easier to place iliosacral screws with the patient
prone. The problems of in-out-in screws I think is related to the supine
position in 2 ways. It is more difficult to get the slightly posterior
to anterior direction that is desirable when the patient is supine. Because
of the increased soft tissue thickness with the patient supine it seems
that all surgeons use canulated screws. I don't like the threaded canula
because it is more flexible than a 3.2 bit and has no feel. The surgeon
using canulated screws relies totally on the x-ray for position. I think
it is safest to use an oscillating drill bit with a pistoning action to
feel the bone. This is what I prefer and feel is safest but certainly
Routt and others have shown good capability to place screws while the patient
is supine. Finally placing the screw seems to occupy quite a bit of discussion but
is really a more minor problem than reducing the fracture. In the future
I think that the table will play a bigger part in the reduction for both
closed and open procedures. I really doubt that currently discussed techniques
such as a Schanz screw in the ilium or manually pulling on the leg can be
consistently effective. The new Pro
FX table from OSI has distal and lateral traction capabilities with
the leg manipulating capabilities of the old Judet Table and has much more
radiolucency than the Judet. This new table will allow 50 degree caudad
and cephalad sacral views. A paradox (to me at least) is that the Pro FX
table will probably also make supine screws easier because the sacrum will
rest on a narrow pedestal rather than the broad table top. Regarding the
problem of reduction we need to consider not only how to move the fractured
side of the pelvis but also how to stabilize the uninjured side to adequately
resist the reduction force. I have come to rely on a device to skeletally
fix the unfractured side of the pelvis to the table which is more effective
in stabilizing the pelvis during traction application than the perineal
post. It largely solves the perineal post problems of deforming the anterior
pelvic ring and allowing rotation around the post. This device (pelvic
stabilizing frame) will also soon be available from OSI. The technique that Chip Routt refers to of prone with an ex fix between
2 tables was shown at a meeting probably 15 years ago but I know of no one
who used it since so one can hardly argue against the prone position based
on this abandoned technique. The ex fix in my opinion has very limited
use for definitive stabilization. For the case shown, I would say that
the ex fix has done its job after the acute period. For definitive fixation
I would remove the ex fix, place the patient prone and reduce and fix the
sacral fracture. Sincerely, Joel Matta
Because of the posterior ring deformity, many surgeons would advocate frame
removal, then roll prone, maintain left sided traction while prone, ORIF
using dorsal exposure, fixation with iliosacral screws and some form of
posterior iliac to posterior iliac fixation (sacral bar, spanning plate, or
screw), then turn supine, assess any residual ring instability, and reapply
the frame or insert a medullary screw if needed. Others would use the
midline exposure for posterior "lumbopelvic fixation" (as described by
Schildhauer) instead.
Others would stay supine, apply some left sided traction to "almost correct"
the ring deformity (it wouldn't be perfect, but almost), adjust the frame as
needed, and insert iliosacral fixation - all done with the patient supine.
I'd likely choose this method, especially if done within the first day or so
after injury in a "sick" patient. His sacrum is competent to accommodate 2
screws based on the CT. Many would advocate long (100-130mm) fully threaded
cancellous iliosacral screws for a sacral fracture. This particular fracture
could be "pushed" a bit with an initial lag screw, then "set" with the
second screw being fully threaded. If you choose to "push" the sacral
fracture, you may consider nerve monitoring during the procedure...take care
if you choose to do this.
Professor-Orthopedic Surgery
Harborview Medical Center
Seattle, WA 98104-2499
Professor-Orthopedic Surgery
Harborview Medical Center
Seattle, WA 98104-2499


