
Date: Wed, 24 Jul 2002 15:24:28 +0200
Subject: Sacroiliac pain after pelvic fracture
From: Dr. Josep M. Muñoz Vives
This 38 yo male suffered a motorbike accident 3 months ago.
He had a past history of AVN of the left femoral head after a hip dislocation, which was treated with a replacement. No other diseases. Hemodynamically stable.
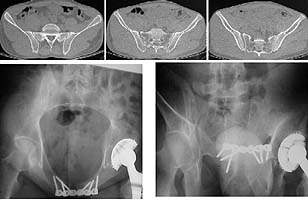
On top row the x-ray and CT the day of admission. Although there was a crack in the posterior ilium this lesion was judged to be an OTA-B1.1. Accordingly, only the pubic symphysis was plated. Post-op x-rays showed reduction of the anterior opening of the sacroiliac joint for what I can recall, because I've been unable to find the x-rays.
Post-op course without complications. He has been allowed sitting and walking with partial weight bearing from the second post-op day.
I saw him last week and he complaints of moderate-severe pain in the gluteal zone with movement, no pain in pubic region.
What would be your opinion?
Should we have fixed the SI joint on admission?
Should we do something now or should we wait to spontaneous fusion?
 |
Dr. Josep M. Muñoz Vives
Orthopedic Dept.
Hospital Universitari Dr. Josep Trueta.
Girona
Catalunya, Spain
Date: Wed, 24 Jul 2002 10:16:34 -0400
From: James Carr
I likely would not have fixed the SI joint if vertically stable as it appears. The "SI" pain may be from persistent instability, but more likely from his lower back e.g. L5-S1. I would manage conservatively. I can't recall ever having made a person better with SI fusion on a late basis, assuming no deformity/nonunion/instability. Chip???
JBC
Date: Wed, 24 Jul 2002 14:37:17 -0700
From: Chip Routt
It's impossible to comment based on these images alone.
Chip
M.L. Chip Routt, Jr.,M.D.
Professor-Orthopedic Surgery
Harborview Medical Center
Seattle, WA 98104-2499
Date: Thu, 25 Jul 2002 10:35:25 +0200
From: Dr. Josep M. Muñoz Vives
Dr. Routt,
Please tell me what data dou you need, clinical or images?
Thanks
Dr. Josep M. Muñoz Vives
Orthopedic Dept.
Hospital Universitari Dr. Josep Trueta.
Girona
Catalunya, Spain
Date: Thu, 25 Jul 2002 07:09:55 -0700
From: Chip Routt
Character and quality of his symptom(s).
Physical findings such as residual instability to exam, focal tenderness, other.
Inlet/outlet pelvic plain films.
Pelvic CT may also be indicated if you truly want to more thoroughly evaluate the patient at this time.
Information is good-
Chip
M.L. Chip Routt, Jr.,M.D.
Professor-Orthopedic Surgery
Harborview Medical Center
Seattle, WA 98104-2499
Date: Fri, 26 Jul 2002 03:06:37 +0200
From: Dr. Josep M. Muñoz Vives
There is no gross instability on physical examination, I've not tested him under image intensification. All tests (Fabere, palpation, hip movement, spine movement...) point to sacroiliac joint. Although not very evident in the images I send, there are clear signs of sacroiliac joint arthritis: Widening, irregularity, esclerosis, possibly cysts and calcification of the capsule. He is waiting a CT scan but I couldn't wait to send the case to the list.
I enclose more images from the preoperative CT and last inlet and outlet.
 |
Dr. Josep M. Muñoz Vives
Orthopedic Dept.
Hospital Universitari Dr. Josep Trueta.
Girona
Catalunya, Spain
Date: Tue, 30 Jul 2002 17:58:09 +0200
From: Dr. Josep M. Muñoz Vives
Yesterday a CT was done, now it becomes clear that the undisplaced sacral and iliac fractures haven't united and probably are the cause of pain. I still question myself about what should be the initial treatmentand which are the predictors of this evolution, because I've seen other patients with similar lesions in the posterior arch whom healed well without fixation. The patient tells me he has been compliant with non weight bearing on the right side.
 |
I also wonder which is the best treatment now, pure transiliac percutaneous fixation oropen debridmentof the pseudoarthrosis with curetage of the sacroiliac joint.
All comments welcome. Thanks in advance.
Dr. Josep M. Muñoz Vives
Orthopedic Dept.
Hospital Universitari Dr. Josep Trueta.
Girona
Catalunya, Spain
Date: Wed, 31 Jul 2002 08:44:40 -0400
From: James Carr
I don't think anything should have been done differently in the initial Rx. I would favor percutaneous sacral screws at this time. It looks like all it needs is stability.
JBC
Date: Wed, 31 Jul 2002 12:31:10 -0700
From: Chip Routt
It's always been helpful for me to view the posterior pelvic ring according to a "three column" concept, similar to that for the spine.
You may find it more helpful in your decision making than any classification scheme.
Examine the imaging studies carefully, and correlate them with your physical examination findings.
For example, use this patient that you've shared with us all. He has a right sided lateral alar fracture, which progresses to (is in continuity with) a posterior iliac fracture...using a "three column" concept, all 3 posterior ring columns are fractured...now it looks analogous to a complete SI joint disruption or complete sacral fracture, yes?
Couple these imaging findings with his unstable exam under anesthesia and fluoroscopy...do you see the mobility of the posterior ring injury as you load the pelvis manually?
So at the first operation given that information, we'd routinely reduce and stabilize his symphysis and then secure the posterior ring lesion with a percutaneously inserted iliosacral screw...lag it if you want , or hold with a fully threaded screw. He has a nice safe zone
At this point, you have several options...further conservative management, other noninvasive bone healing modalities (electrical stimulation or other), percutaneous fixation, or open debridement-reduction-fixation.
If he's still symptomatic posteriorly, I'd advocate percutaneous stability using first an iliosacral lag screw to compress the lesion, followed by a second fully threaded iliosacral screw to secure the compression and help resist rotary mobility. That will work.
You should closely follow his anterior plate also...it's "working overtime" right now, and soon to fail in some mode...according to your plain films, the symphysis is already distracted slightly. Check an xray right before he's anesthetized...that plate may have failed by then! He'll know before you will...he'll feel pain and "grinding" several inches deep, between scrotum and rectum...he'll tell you (even if you don't ask) when it happens.
Try the 3 column concept for your posterior pelvic ring injuries...it won't fail you.
Chip
M.L. Chip Routt, Jr.,M.D.
Professor-Orthopedic Surgery
Harborview Medical Center
Seattle, WA 98104-2499
Date: Fri, 2 Aug 2002 05:56:05 -0700
From: Zsolt Balogh
What are the three columns of the posterior pelvic ring ?
Thank you,
Zsolt Balogh
Date: Tue, 13 Aug 2002 03:03:20 +0200
From: Josep M. Muñoz Vives
I've followed list advice and decided to fix the sacroiliac joint but checked first the plate and it didn't seem to have moved. Here is the initial result. Postop the patient feels that his buttock is 'stronger' which is a common finding after sacroiliac fixation. His pain is much better. I'll keep the list posted about the end result. Thanks to everyone for nice advice and explanation which will be in my mind for further cases.
Dr. Josep M. Muñoz Vives
Orthopedic Dept.
Hospital Universitari Dr. Josep Trueta.
Girona
Catalunya, Spain
Date: Tue, 13 Aug 2002 06:42:14 -0700
From: Zsolt Balogh
Can anybody let me know, what is the three column theory for the posterior pelvic ring (analogous to the spine)? What are the three columns in the posterior ring?
Thanks,
Zsolt Balogh, MD
Date: Tue, 13 Aug 2002 2:00 PM EST
From: Bill Burman
Zsolt
Chip Routt phoned this am. He is away on vacation but somehow your message got
through. Your 3-column question (and perhaps computer withdrawal) are not
permitting him to rest so he has asked me to convey the following explanation
until he returns:
Looking at the axial CT, the middle column of the posterior pelvic ring extends
from the anterior aspect of the sacral foramina to the posterior cortex of the
sacral body or the anterior limit of the sacral spinal canal. The anterior column
includes anything anterior to the middle column to the extent of the anterior
pelvic ring. The posterior column includes anything posterior to the middle
column to the extent of the posterior iliac crest.
There are no formal studies which establish the clinical significance of this
classification system. It is only anecdotal at this stage. While the clinical
significance of the 3 column spinal injury classification has been called into
question e.g.
John Sledge's OTA
Basic Fracture Course Lecture
Chip Routt says there is a very close correlation with a disruption of the 3
columns of the posterior pelvis as was seen on consecutive axial CT cuts in this case
and clinically significant posterior pelvic instability.
Bill Burman, MD
Date: Wed, 14 Aug 2002 00:26:28 +0530
From: DR T I GEORGE
I have a question to the experts in these type of injuries.
In this case the sacro-iliac joint has been stabilised with two screws. This
is a late stabilisation much after the injury. As far as I can make out no
fusion has been done. This means the stability of the sacroiliac joint is
dependent on the two screws or in other words till the metalware fails since
there is no scope for biology to stabilise this area in the absence of a formal
fusion. I will be thankful if someone can clarify whether this late
stabilisation needs formal fusion for biology to take over before the implants
fail. If there is no need for fusion I will be thankful for an explanation.
DR T I GEORGE,
Date: Sat, 17 Aug 2002 23:39:38 +0200
From: Josep M. Muñoz Vives
Dr. George:
I'm not an expert and that was my doubt too. I can be wrong, but I expect the
screws to stabilize the sacral and iliac fractures until they heal and that this
will be enough, because in this case the posterior ligaments are not so disrupted
as in a true sacroiliac dislocation so it is more a fracture instability than a
joint instability. So once the sacral and the iliac fractures consolidate the
joint will be no longer unstable. I agree with you that once the fracture
is healed there still will be two screws crossing a joint whith a potential for
screw breakage. I expect as you a comment from the experts but I understand
they also have the right to rest.
Dr. Josep M. Muñoz Vives
From: Chip Routt
Date: Tue, 20 Aug 2002 11:39:06 -0700
The injury of the posterior pelvic ring was a fracture displaced through the
sacrum, a portion of the SI ligamentous zone/area, and posterior ilium.
The instability likely caused persistent and worsening symptoms.
The initial lag screw provides compression of the "incomplete/delayed union",
and the second fully threaded screw provides another fixation point to diminish
local fracture motion and support the compression delivered by the initial lag
screw...in theory.
The goals are to diminish fracture motion to promote eventual/completed
fracture healing, and diminished symptoms/complaints.
After iliac and sacral fracture unions, the screws have no function. Some
surgeons recommend iliosacral screw removal...have a good day if you choose that
road!
The articular relationship of the SI joint is not affected by this particular
injury, at least as it has been shared in the imaging studies.
Proper screw starting point, orientation, length, and function will not
disturb the SI articular relationship.
After such fixation, the associated symptoms resolve, the fractures heal, the
SI articular relationship is preserved, the patient returns to work.
It's very rare to see well positioned standard 7mm AO/ASIF cannulated
iliosacral screw fatigue failure by "screw-breakage". Noncannulated standard
6.5mm cancellous screws did demonstrate such failure.
More commonly, at long term follow up the pelvic radiographs reveal subtle
local screw changes such as 1-2mm disengagement, especially in those patients
with normal SI appearance...reflective of unimpaired SI mobility, perhaps.
In others, consolidation of the SI joint occurs (for whatever reason) and the
screws show no positional changes.
These details are dependant on many factors.
There are so many details for what seem to be simple screws...but the details
are the keys.
Chip
M.L. Chip Routt, Jr.,M.D.
image adapted from - Routt ML Jr, Simonian PT; Posterior Pelvic Ring
Disruptions.; Chapt 37 Master techniques of orthopaedic surgery: Fractures; ed
Wiss D; Lippincott-Williams & Wilkins, 2000

HWB Foundation
Consultant Orthopaedic surgeon,
Polytrauma, Microvascular and Hand Surgery Unit,
Metropolitan Hospital, Trichur, South India.
Orthopedic Dept.
Hospital Universitari Dr. Josep Trueta.
Girona
Catalunya, Spain
Professor-Orthopedic Surgery
Harborview Medical Center
Seattle, WA 98104-2499